For pharmaceutical, food, and medical device companies, staying compliant with FDA regulations is a constant challenge. Even minor oversights can result in serious consequences. One of the most severe outcomes is receiving a consent decree from the FDA, which can lead to production shutdowns, hefty fines, and long-term reputational harm. During this period, businesses may face operational restrictions, mandatory third-party oversight, and frequent FDA inspections. Noncompliance with the decree can bring even harsher penalties.
To avoid the risks associated with a consent decree FDA, companies need to stay ahead of regulatory issues. In this blog, we’ll explain what an FDA consent decree means, how it affects your operations, and what you can do to protect your business.
TL;DR
- Overview of what the FDA consent decree is and how it impacts business.
- It significantly impacts business operations, potentially leading to operational shutdowns.
- Common triggers include persistent cGMP failures, ignored Form 483s, unaddressed FDA warning letters, and ongoing public health risks.
- It typically follows repeated noncompliance, indicating systemic quality issues and a failure to adequately respond to prior regulatory actions.
What Is a Consent Decree?
A consent decree is a legally binding agreement between the FDA and a company that has failed to comply with regulatory standards. It acts as a final opportunity for the company to correct serious violations before facing litigation or being shut down. The consent decree outlines specific corrective actions and timelines, which are verified by a third-party monitor.
Consent decrees derive their power from the Federal Food, Drug, and Cosmetic Act (FDCA). In 1999, Congress granted the FDA enhanced authority to enforce compliance by garnishing profits from companies that repeatedly fail to address quality system nonconformances.
Once under a consent decree, your business will face strict oversight, audits, and financial penalties for every day you fail to comply. These agreements often last five years or more and come with extensive legal and operational obligations.
Key points about FDA consent decrees:
- It is a negotiated agreement between the company and the FDA, often filed in U.S. District Court and signed by top company officials, the U.S. Attorney, and the Court.
- The decree details voluntary corrective actions the company must take to remedy violations and improve its systems, particularly quality management and cGMP compliance.
- Consent decrees are usually the result of repeated nonconformance, such as:
- Multiple FDA Form 483 observations across audits
- Ignored or insufficient responses to FDA warning letters
- Lack of a defined plan to correct recurring GMP issues
- It is designed to change the company’s compliance culture by pulling it out of a pattern of long-standing quality failures.
- Companies under consent decrees must undergo third-party oversight to ensure that improvements are completed on time and meet FDA standards.
- While restrictive, consent decrees often allow the company to continue operating under strict conditions, ensuring that product quality is not compromised for consumers.
Why do Consent Decrees Matter?
Consent decrees can carry severe consequences for companies. Sometimes, it even results in a permanent shutdown. For example, in 2018, Cantrell Drug Company, a sterile compounding facility, entered into a consent decree with the Department of Justice, which required it to cease operations until it addressed regulatory violations and demonstrated full compliance with current good manufacturing practices (cGMP).
- Cantrell achieved compliance within five months.
- However, the operational and financial disruption was already too great.
- The company filed for bankruptcy shortly after, despite remediation efforts.
This case illustrates how even a short-term disruption under a consent decree can have fatal consequences for a business.
What Triggers a Consent Decree?
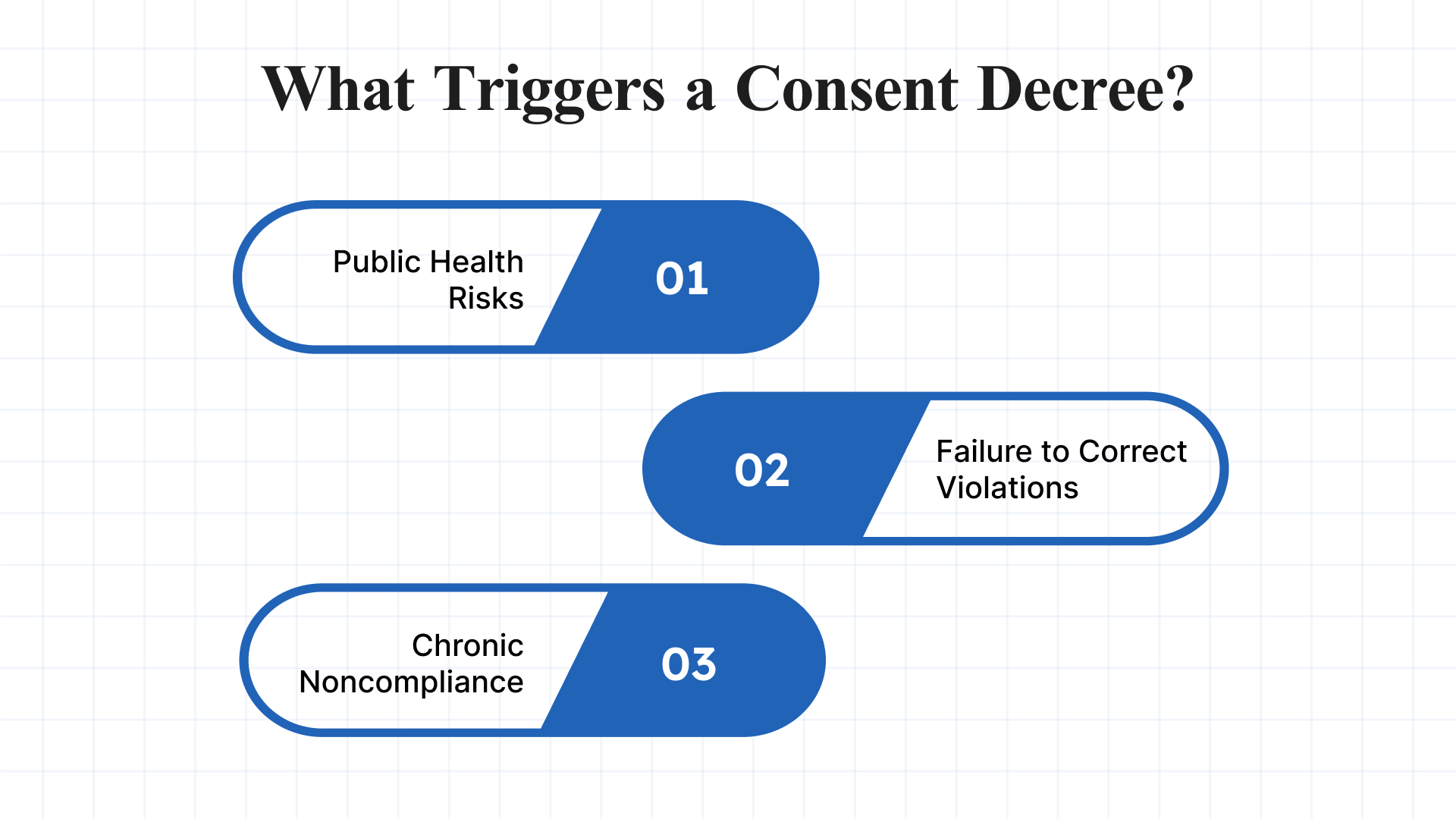
The FDA typically seeks injunctions and consent decrees when voluntary compliance efforts have failed or when public health is at risk. These legal actions are not taken lightly and usually follow a pattern of serious, repeated, or unaddressed violations.
Common Triggers Include:
- Public Health Risks: The presence of serious safety threats, such as product contamination, adulteration, or the potential for patient harm, can prompt immediate legal action. This is especially true in cases involving sterile drug products, medical devices, or food production.
- Failure to Correct Violations: If a company repeatedly violates FDA regulations and fails to adequately respond to Warning Letters, Form 483s, or untitled letters, the FDA may escalate to legal enforcement. A pattern of non-responsiveness or inadequate remediation is a major red flag.
- Chronic or Egregious Noncompliance: Longstanding or egregious violations, especially those that suggest weak internal controls, poor quality systems, or management negligence. It may indicate that the company is unable or unwilling to operate within regulatory expectations.
Common Types of Violations That Lead to Consent Decrees
Consent decrees are typically the result of serious and sustained regulatory violations. Below are some of the most common types of issues that prompt this level of enforcement:
- Noncompliance with Current Good Manufacturing Practices (cGMP): Includes issues such as inadequate sterility assurance, cross-contamination risks, poor documentation practices, or failure to validate manufacturing processes.
- Distribution of Unapproved or Misbranded Drugs: Marketing or distributing drugs without proper FDA approval or failing to meet labeling requirements can result in swift enforcement action.
- Insanitary or Unsafe Production Conditions: Facilities found to have pest infestations, unsanitary equipment, or improper cleaning procedures are subject to heightened scrutiny and potential injunction.
- Data Integrity Violations: Manipulation, deletion, or falsification of records (particularly in quality control or testing labs) significantly undermines regulatory trust and is often cited in enforcement actions.
- Failure to Investigate Product Complaints or Deviations: Companies that fail to properly investigate adverse events, product defects, or manufacturing deviations may be perceived as failing to protect patient safety.
Also read: Effective FDA Form 483 Response Strategies
How to Respond to a Consent Decree FDA?
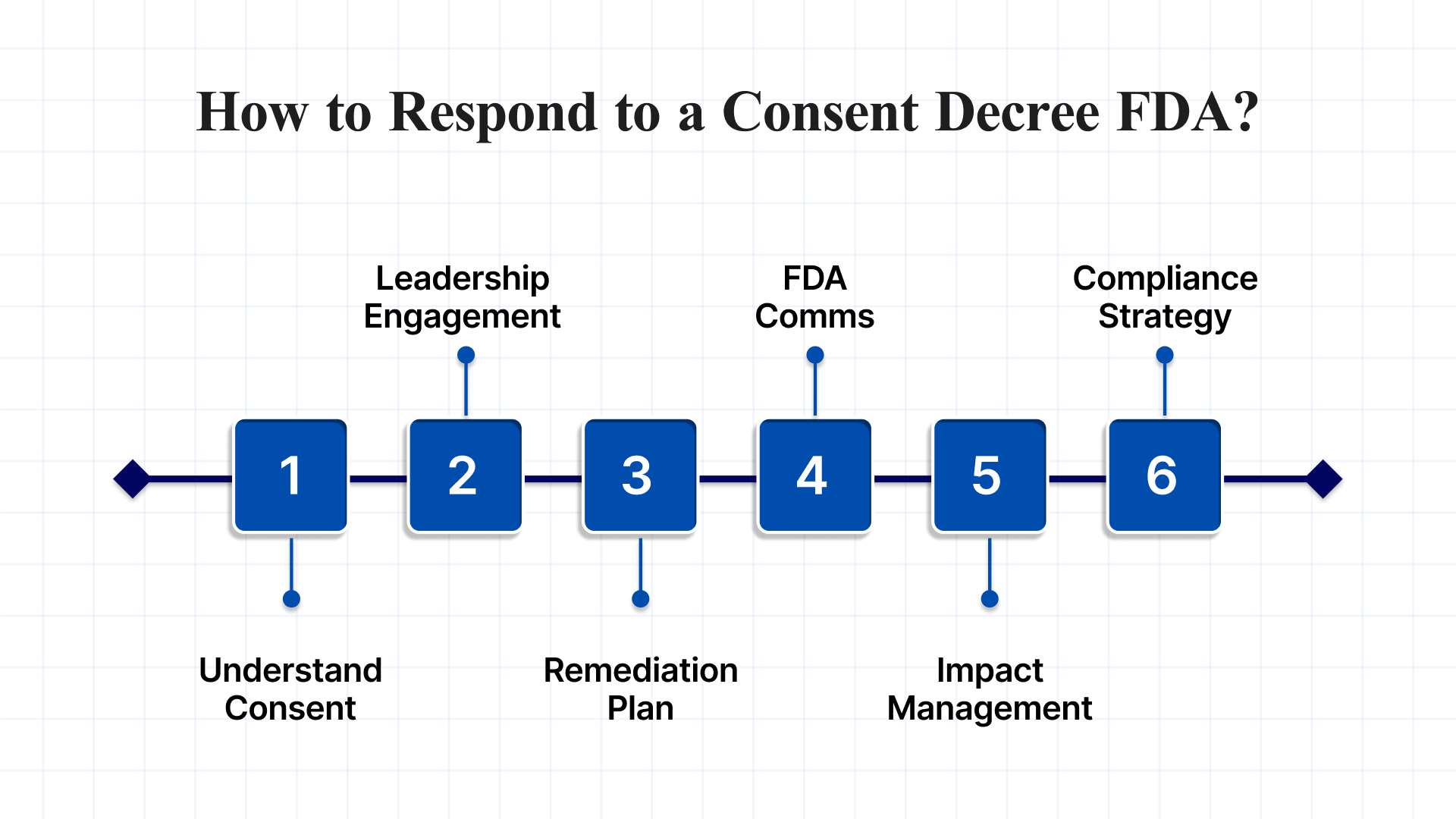
Responding effectively to an FDA consent decree requires a strategic, comprehensive, and disciplined approach, as these are serious legal agreements that impose strict corrective actions and ongoing oversight. Here are the key steps and best practices to respond to and manage a consent decree based on expert guidance and real-world cases:
1. Understand the Consent Decree Fully
- Review all documents carefully: Understand the specific violations cited, the corrective actions required, timelines, financial penalties, and reporting obligations.
- Recognize it is a court order: The consent decree is legally binding and often results from repeated failures to address FDA observations over time, so it is not a surprise but a culmination of prior enforcement actions like Form 483s and warning letters.
2. Engage Senior Management and Legal Counsel
- Top management commitment: Senior leadership must take ownership and demonstrate accountability, as the decree often requires the signature of the company’s highest official and involves naming responsible officers.
- Work closely with FDA-experienced legal counsel: To negotiate terms, ensure compliance with legal requirements, and manage communications with the FDA and courts.
3. Develop and Implement a Robust Remediation Plan
- Conduct thorough gap analyzes and root cause investigations: Identify systemic issues underlying the violations and develop Corrective and Preventive Actions (CAPA) with clear timelines.
- Facility and process upgrades: This may include equipment qualification, computer system validation, improved change control, and enhanced laboratory investigations to meet cGMP standards.
- Third-party oversight: Consent decrees often require independent third-party auditors or consultants to verify compliance and sometimes to perform lot release or certification functions.
4. Maintain Transparent and Timely Communication with FDA
- Regular reporting: Submit detailed progress reports as required, including evidence of completed corrective actions and any challenges encountered.
- Engage proactively: Schedule meetings with FDA representatives to clarify expectations and demonstrate commitment to compliance.
5. Manage Production and Business Impact
- Comply with production restrictions: Some products may need to be halted or recalled until remediation is complete, and new product launches may be delayed.
- Plan for financial impacts: Be prepared for fines and liquidated damages for missed deadlines, and factor remediation costs into business planning.
6. Prepare for Long-Term Compliance and Exit Strategy
- Sustain improvements: The company must maintain compliance over a period (often years) and demonstrate this to petition for lifting the decree.
- Culture change: Use the consent decree as an opportunity to embed a culture of quality and compliance throughout the organization.
Business and Financial Impact of Consent Decrees
The consequences of FDA consent decrees go far beyond regulatory compliance. They can profoundly impact a company’s financial health, reputation, and long-term viability.
In 1999, the FDA was granted authority by Congress to garnish profits from companies with recurring quality system violations. As Lester Crawford, then deputy commissioner of the FDA, warned:
“Manufacturers who choose to wait until FDA investigators find violations, rather than policing themselves, will find that they have made a poor and costly decision.”
This has proven true across the pharmaceutical industry. Of the sixteen companies that received consent decrees, five were sold or acquired afterward—Steris, Centeon, Biocraft, W-T, and Pennex—suggesting serious business ramifications tied to regulatory issues.
Case Study: Abbott
Few examples illustrate the full weight of a consent decree like Abbott.
In its 1999 Annual Report, Abbott disclosed a staggering $168 million one-time charge due to a consent decree, which included:
- $100 million in fines paid to the FDA
- $44 million for contractual obligations
- $24 million in unusable inventory
These costs were just the beginning. By 2000, Abbott estimated the decree had reduced sales by $250 million, and total losses were projected to exceed $1 billion by 2003.
The ripple effects extended to strategic growth: Abbott’s proposed $7.3-billion acquisition of Alza fell through, an indirect consequence of the decree that damaged investor confidence and shifted internal focus toward remediation over expansion.
The financial burden didn’t stop there:
- In 2002, Abbott wrote off $140 million, covering quality efforts, market erosion, and canceled product launches.
- Another $112 million fine followed after a failed follow-up inspection.
- Abbott conducted 14 massive process validation studies, each averaging 6,000 pages and totaling 60,000 man-hours, costing around $126 million.
- The company completed 250+ product-specific validations (2.6 million hours), totaling another $350 million.
- Over 1,500 employees required retraining.
This example shows how a single decree can derail operations, stall innovation, and burn hundreds of millions in corrective measures.
How Atlas Compliance Helps You Avoid FDA Consent Decrees
An FDA consent decree is one of the most disruptive and expensive enforcement actions a company can face. These legally binding agreements often result in halted operations, multi-million-dollar fines, and years of third-party oversight. To avoid reaching that point, companies must be proactive, identifying compliance gaps before the FDA does.
Atlas Compliance is the leading FDA inspection intelligence platform, purpose-built to help pharmaceutical and life sciences companies stay compliant and inspection-ready, ultimately reducing the risk of enforcement actions like consent decrees.
- Turn FDA enforcement data into preventive action: We analyzes decades of FDA data, including Form 483s, warning letters, CFR citations, and consent decree trends, to give you real-time visibility into compliance risks.
- This intelligence allows you to proactively address potential issues before they escalate into costly legal action.
- Comprehensive inspection insights: Access FDA inspection data dating back to 2004, including outcomes, citations, and enforcement patterns.
- Weekly updates ensure you stay current with the latest inspection trends and enforcement activities.
- Identify red flags that have led to past consent decrees across your industry.
- AI-driven search and analysis: Use natural language processing (NLP) to quickly analyze complex FDA documents like 483s, warning letters, and inspection reports.
- Understand patterns in inspector behavior and citation frequency to better prepare your facilities.
- Spot early indicators of noncompliance that could lead to serious regulatory consequences.
- Predictive analytics & machine learning: We utilize machine learning to identify emerging inspection trends and high-risk operational areas.
- Prioritize quality initiatives based on real enforcement data.
- Avoid surprises by anticipating how your facility or product line might be viewed by regulators.
- Cross-industry oversight & supply chain management: Go beyond human drugs: monitor FDA enforcement across biologics, vaccines, food, cosmetics, and more.
- Evaluate supplier compliance and avoid risk by partnering with vendors who meet FDA expectations.
- Protect your business from becoming collateral damage in a partner’s consent decree.
Conclusion
FDA consent decrees are a serious matter for any company in the pharmaceutical, food, or medical device industries. The consequences of a consent decree can be severe, ranging from operational shutdowns to significant fines and reputational damage. By staying proactive and utilizing advanced compliance tools like Atlas Compliance, your business can avoid the risks of noncompliance, ensure regulatory readiness, and avoid the need for costly corrective actions.
Book a Free Demo Todayand see how Atlas Compliancecan help you detect issues early, streamline documentation, and maintain continuous compliance.
FAQs
Q1. What is a Consent Decree by the FDA?
A1. A Consent Decree is a legally binding agreement between the U.S. Food and Drug Administration (FDA) and a pharmaceutical or medical device company. It is typically issued when the FDA identifies significant violations, such as breaches of Good Manufacturing Practices (GMP), and the company has failed to adequately correct them. The decree outlines specific corrective actions and is enforced by a federal court.
Q2. What is the Purpose of a Consent Decree?
A2. The main purpose of a consent decree is to resolve regulatory violations without a formal trial, while ensuring that the company takes legally enforceable steps to correct the issues. It acts as a court-supervised improvement plan and often includes provisions for process changes, independent monitoring, and long-term compliance reporting. It does not require an admission of guilt, but the consequences for noncompliance are significant.
Q3. How Long Do FDA Consent Decrees Last?
A3. FDA consent decrees typically remain in effect until the company demonstrates sustained compliance over several years, most commonly five consecutive years. However, the duration may vary depending on the severity of the violations and the company’s responsiveness. The decree is lifted only after a thorough review confirms full and consistent adherence to regulatory standards.
Q4. What is the Difference Between a Consent Agreement and a Consent Decree?
A4. A Consent Agreement is a private, enforceable contract between a company and a government agency. It is not filed in court, but violations can still carry legal consequences. On the other hand, a Consent Decree, by contrast, is a formal court order, typically the result of litigation or a negotiated settlement. It carries the full weight of the judicial system and is enforceable through the courts, including penalties for noncompliance.
