Ensuring quality and compliance in the pharmaceutical industry is more challenging than ever. Companies face increasing regulatory scrutiny, complex global supply chains, and pressure to avoid quality issues that risk patient safety or delay production. A major weak point is the supplier network, where unqualified suppliers can cause violations, poor materials, and costly recalls.
However, managing complex regulations, maintaining strict quality standards, and controlling supplier risks that could impact product integrity and brand reputation can be incredibly challenging.
To address these risks, pharmaceutical companies need a proactive supplier qualification strategy. This involves thoroughly evaluating suppliers for quality, compliance, and performance. A strong qualification process helps reduce risk, ensure regulatory alignment, and strengthen supply chain reliability.
This blog explores how to effectively ensure the quality of your suppliers in the pharmaceutical industry.
Key Takeaways:
- Overview of how supplier qualification ensures pharma companies meet regulatory and quality standards.
- Key regulations include FDA 21 CFR, ISO 13485, GMP, GDP, and ICH guidelines, all of which mandate documented evaluations, risk controls, and traceability.
- The process involves multiple steps—from pre-screening and risk assessment to audits, quality agreements, and performance monitoring.
- Products requiring qualification include APIs, reagents, medical device components, and packaging materials that affect drug safety and efficacy.
- A risk-based approach is essential, with higher scrutiny applied to suppliers that pose greater quality or compliance risks.
What is Supplier Qualification?
Supplier Qualification (SQ), also known as Vendor Qualification (VQ), is the process of assessing, selecting, and approving suppliers, vendors, or contractors to confirm they can consistently deliver goods or services that meet a company’s quality and compliance standards.
This process is vital in ensuring that suppliers can provide the materials, components, and services needed for pharmaceutical products while adhering to strict regulatory requirements such as Good Manufacturing Practices (GMP) and Good Distribution Practices (GDP).
It ensures that the materials, components, and services meet strict regulatory requirements. Devices and raw materials conform to quality and safety standards. Supplier qualification is critical in life sciences industries, including: Pharmaceuticals, Biotechnology, and Medical devices.
Key Regulations Followed by the Pharma Industry for Supplier Qualification
The pharmaceutical industry is one of the most highly regulated sectors in the world, and supplier qualification is closely linked to several critical regulatory frameworks. Suppliers in the pharma space must comply with regulations from various bodies such as the FDA, ISO, and ICH to ensure that they are producing high-quality products
| Standards | Key Requirements |
| ISO 13485 | Risk-based controls, quality agreements, and traceability for medical devices |
| FDA 21 CFR 820 | Documented evaluation procedures and change notifications |
| GMP/GDP | Validated processes, audit trails, and supply chain integrity |
| ICH Q10 | Pharmaceutical supply chain oversight and quality metrics |
Here are some of the key regulations governing supplier qualification:

- FDA (Food and Drug Administration): Ensures that pharmaceutical products meet rigorous safety and quality standards.
- ISO 13485: Specifies requirements for a quality management system where an organization needs to demonstrate its ability to provide medical devices and related services.
- GMP (Good Manufacturing Practices): Provides guidelines on the conditions and practices under which pharmaceutical products should be produced and controlled.
- GDP (Good Distribution Practices): Focuses on the proper distribution and transportation of pharmaceutical products.
- ICH (International Council for Harmonization): Develops global guidelines on pharmaceutical standards and ensures the safety, quality, and efficacy of medicines.
Importance of Supplier Qualification
Supplier qualification is crucial for maintaining a consistent and compliant supply chain. Here are some reasons why supplier qualification is essential:
- Regulatory Compliance: Ensures that suppliers meet the regulatory requirements for the pharmaceutical industry.
- Risk Mitigation: Identifies potential risks from suppliers early on, including compliance violations, delays, or quality control issues.
- Product Quality: Ensures that the raw materials, components, and services supplied meet the necessary standards of quality, preventing defects in the final product.
- Operational Efficiency: Streamlines procurement processes by working with suppliers that are already qualified, leading to fewer disruptions in production schedules.
Step-by-Step Guide: Supplier Qualification Process
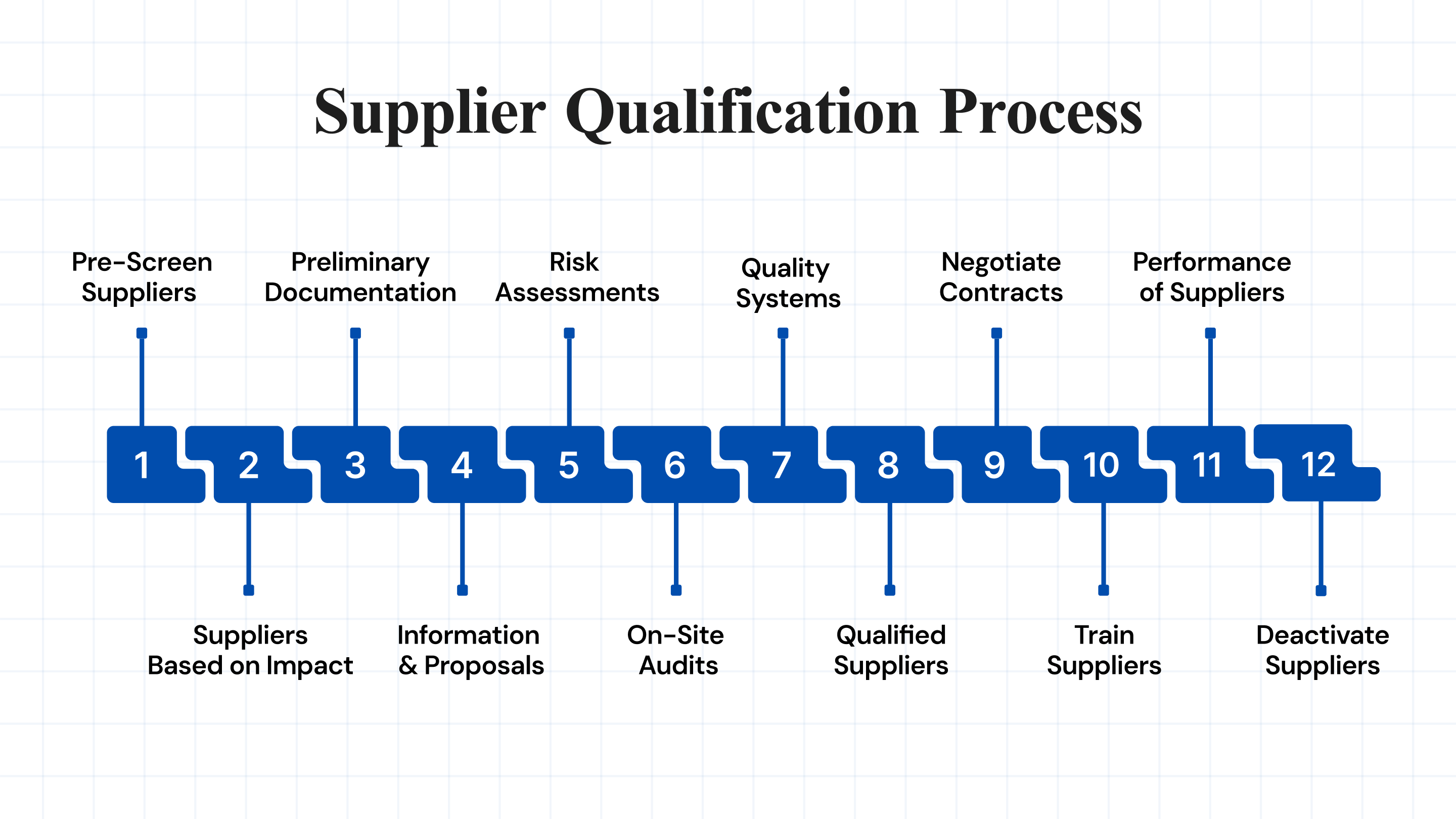
The supplier qualification process typically involves the following steps:
1. Identify and Pre-Screen Suppliers
Begin the supplier qualification process by identifying and screening potential vendors to ensure alignment with your quality, compliance, and operational requirements.
- Conduct market research using databases, directories, and regulatory resources.
- Review supplier portfolios to confirm product/service compatibility.
- Evaluate reputation through past performance, reviews, and testimonials.
- Assess financial health via statements and credit risk ratings.
- Analyze operational capacity, including production volume and consistency.
- Verify certifications and compliance with local and global regulations.
2. Classify Suppliers Based on Impact
Classify suppliers according to their influence on product quality and regulatory obligations to support a risk-based qualification strategy.
- Categorize suppliers as either quality-critical or standard.
- Identify quality-critical suppliers providing high-impact materials/services.
- Apply stricter controls, audits, and monitoring for critical suppliers.
- Standard suppliers require less intensive qualification due to minimal risk.
3. Gather Preliminary Documentation
Collect essential documents early to eliminate non-compliant vendors and reduce evaluation time and risk.
- Request company profiles, licenses, certifications, and compliance documents.
- Verify cGMP, ISO 13485, and other relevant certifications.
- Confirm international compliance, including FDA letters.
- Use qualification questionnaires to assess QMS, past audits, and risk management.
- Analyze incident history and previous performance records.
4. Request Information and Proposals
Gather detailed proposals to compare suppliers across compliance, technical capability, cost, and service delivery.
- Define and communicate project scope, quality expectations, and compliance needs.
- Use RFI to gather general capabilities and market info.
- Use RFP for technical, financial, and operational evaluations.
- Use RFQ for pricing, terms, and lead-time clarity.
- Compare responses against compliance, cost, and supply chain fit.
5. Conduct Risk Assessments
Evaluate potential risks related to quality, compliance, and supply continuity to prevent disruptions.
- Identify risks from supplier audits, complaint history, and delivery reliability.
- Review past performance and incident trends for early warning signs.
- Evaluate compliance risks tied to FDA, cGMP, and ISO standards.
- Consider financial and operational risks such as production bottlenecks.
6. Perform On-Site Audits
On-site audits verify supplier practices and regulatory adherence, ensuring alignment with your quality standards.
- Plan the audit scope and checklist based on supplier classification.
- Inspect production workflows, sanitation, equipment, and traceability.
- Interview staff and evaluate SOP compliance.
- Document non-conformities and enforce corrective actions.
- Schedule routine re-audits for continuous oversight.
7. Review Quality Systems and Documentation
A detailed review of a supplier’s quality documentation validates process control, traceability, and regulatory readiness.
- Examine SOPs, quality manuals, batch records, and validation protocols.
- Confirm documentation accuracy, completeness, and relevance.
- Evaluate change control procedures for equipment or material updates.
- Assess traceability from raw material sourcing to product release.
8. Approve Qualified Suppliers
Formally approve suppliers that meet all regulatory, quality, and business criteria, adding them to your Approved Supplier List (ASL).
- Compile audit results, risk data, and quality verification.
- Validate that the supplier meets all compliance and performance standards.
- Include approved suppliers in the ASL as authorized vendors.
- Regularly review and update the ASL to ensure ongoing compliance.
9. Negotiate Contracts and Quality Agreements
Establish clear expectations through contracts and quality agreements to define roles, responsibilities, and compliance obligations.
- Draft quality agreements outlining metrics, CAPA, and audit schedules.
- Define pricing, delivery terms, confidentiality, and dispute resolution.
- Align both parties on performance standards and regulatory requirements.
- Schedule periodic reviews to ensure agreement relevance.
10. Onboard and Train Suppliers
Effective onboarding and training ensure that suppliers understand requirements and align with operational and regulatory needs.
- Integrate suppliers into procurement and quality systems.
- Communicate expectations on documentation, delivery, and compliance.
- Provide training on QMS, CAPA, and audit preparedness.
- Maintain open communication to monitor and support performance.
11. Monitor and Manage the Performance of Suppliers
Ongoing performance monitoring ensures continued compliance and helps prevent issues before they impact operations.
- Inspect received products for conformity and quality.
- Use KPIs and scorecards to track delivery, quality, and satisfaction
- Conduct re-audits and periodic performance evaluations.
- Initiate CAPA for significant issues and monitor resolution progress.
12. Requalify or Deactivate Suppliers
Regularly reassess suppliers to ensure continued compliance or remove those who pose quality or regulatory risks.
- Perform scheduled audits and risk evaluations.
- Provide feedback for continuous improvement and collaboration.
- Define and enforce deactivation criteria for underperforming vendors.
- Remove non-compliant suppliers to maintain product integrity and safety.
Using advanced platforms like Atlas Compliance can simplify this process. Atlas provides comprehensive access toFDA inspectionreports, 483s, warning letters, and CFR citations, helping you to assess suppliers effectively and stay ahead of any potential risks.
What are the Products and Services Requiring Supplier Evaluations in Pharma?
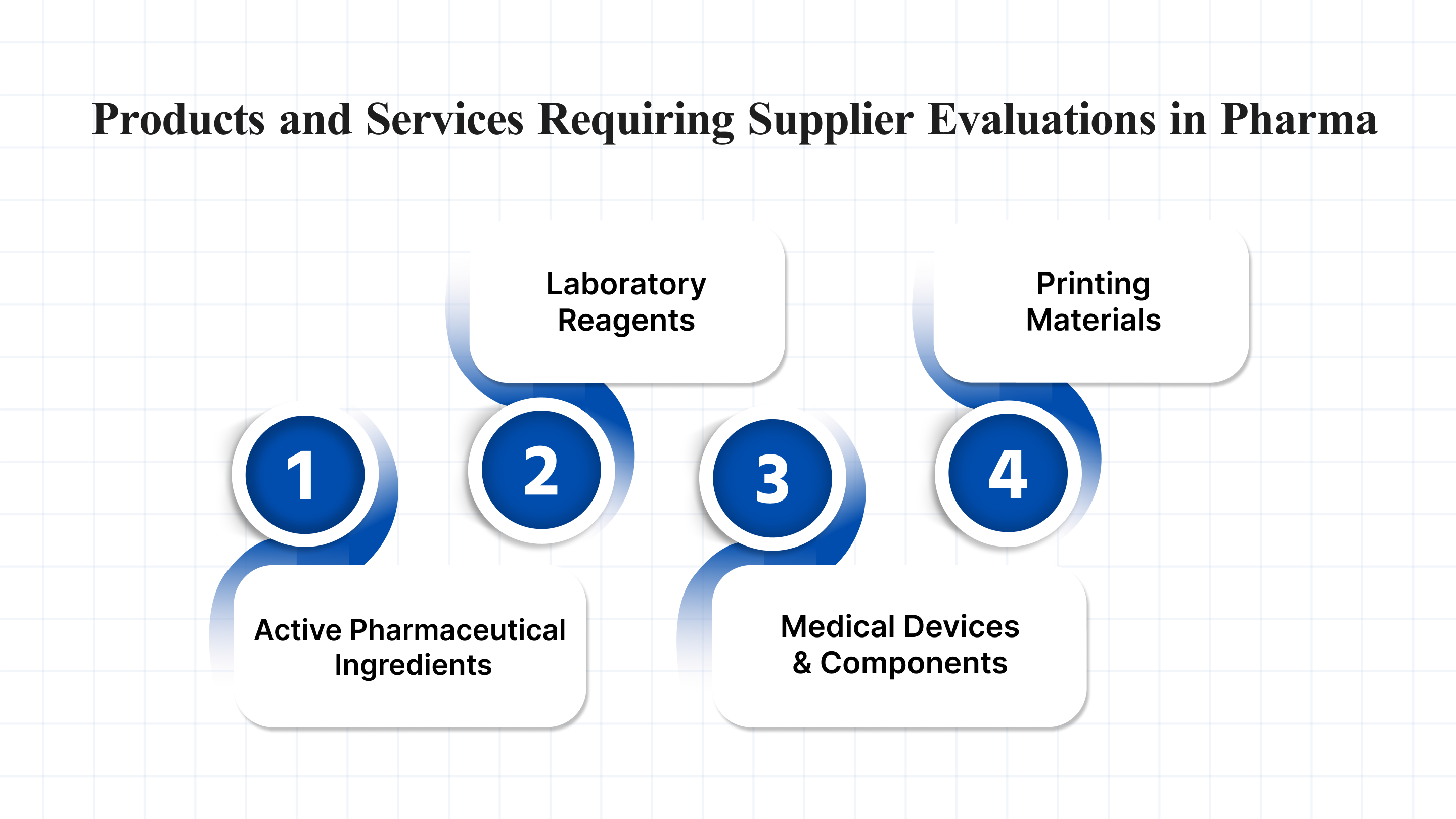
In the pharmaceutical industry, products and services that directly or indirectly impact drug safety, efficacy, or regulatory compliance are considered quality-critical. These must be sourced from suppliers who meet rigorous evaluation criteria, including adherence to regulatory standards, strong quality management systems, and effective risk mitigation strategies.
Below are examples of quality-critical products in the pharmaceutical industry that require thorough supplier evaluation:
- Active Pharmaceutical Ingredients (APIs): APIs must be sourced from suppliers that comply with ICH Q7 guidelines, demonstrating adherence to GMP standards, raw material traceability, and measures to prevent contamination or cross-contamination.
- Laboratory Reagents and Consumables: Laboratory reagents should come from ISO 17025-accredited suppliers and must be validated for use in GLP- or GMP-compliant environments.
- Medical Devices and Components: Suppliers of medical devices and components should follow ISO 13485 standards and comply with FDA 21 CFR Part 820 (Quality System Regulation) to ensure quality and regulatory alignment.
- Packaging, Labeling, and Printing Materials: Suppliers must comply with FDA 21 CFR Part 211 and applicable UDI requirements. They should also implement serialization and tamper-evident features in line with DSCSA and relevant market-specific regulations.
Each of these areas requires careful supplier qualification to ensure compliance and quality.
Guidelines and Requirements for Supplier Qualification
Supplier qualification requirements ensure vendors comply with regulatory, quality, and operational standards before being approved for sourcing.
Below are the key supplier qualification requirements in the Pharma industry.
GDP Supplier Qualification Requirements
The Good Distribution Practices (GDP) guidelines ensure that pharmaceutical products are stored, transported, and handled appropriately. Supplier qualification in GDP focuses on evaluating the supplier’s ability to maintain product integrity during distribution and to comply with temperature control and security standards.
GMP Supplier Qualification Requirements
The Good Manufacturing Practices (GMP) guidelines ensure that pharmaceutical products are consistently produced and controlled to the highest quality standards. Supplier qualification in GMP involves ensuring that suppliers meet requirements for cleanrooms, equipment, production processes, and personnel qualifications.
FDA Supplier Qualification Requirements
FDA regulations, specifically 21 CFR Part 210 and 211, outline the standards for manufacturing, processing, packaging, or holding drugs. Suppliers must demonstrate adherence to these standards, ensuring that products meet the FDA’s quality and safety criteria.
ISO 13485 Supplier Qualification Requirements
ISO 13485 sets the criteria for quality management systems in the design and manufacture of medical devices. Suppliers involved in providing materials or services for medical devices must be qualified against these standards to ensure regulatory compliance.
ICH Supplier Qualification Requirements
The International Council for Harmonization (ICH) sets global guidelines for pharmaceutical manufacturers. Supplier qualification must adhere to these guidelines, ensuring that materials and components used in pharmaceutical production meet international standards.
Best Practices for Risk-Based Supplier Performance Monitoring
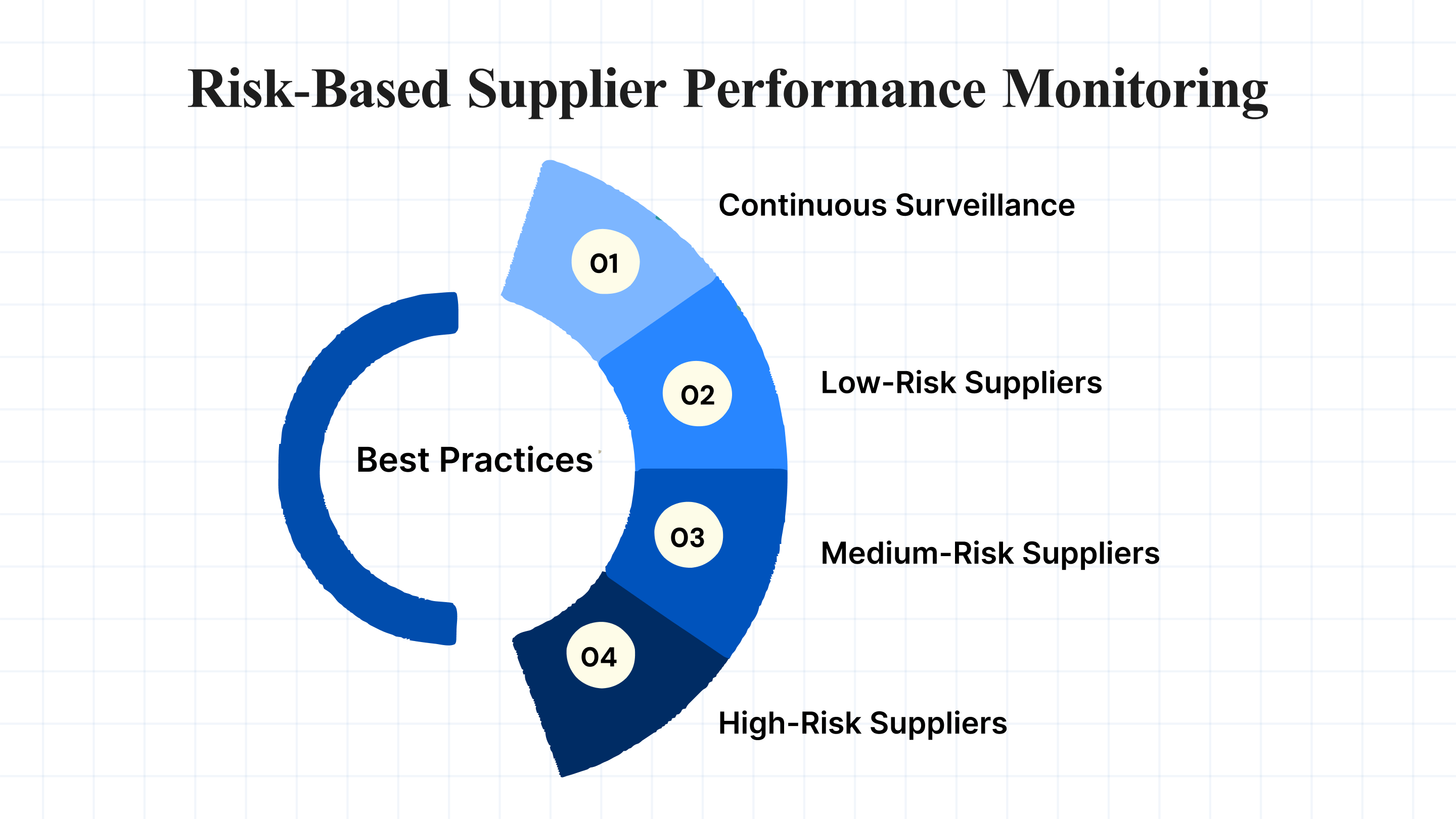
Risk-based monitoring involves assessing and tracking potential risks across the supply chain and adjusting supplier qualification efforts based on these risks. Key strategies include:
- Continuous Surveillance: Use advanced platforms like Atlas Compliance to monitor regulatory changes and inspection outcomes across suppliers. This ensures that companies are always aware of any compliance risks.
- Low-Risk Suppliers: Conduct basic due diligence using supplier questionnaires to evaluate capabilities, financial health, and compliance with relevant standards. Monitor performance through regular reviews and reporting to detect any emerging risks.
- Medium-Risk Suppliers: Apply structured audits, track key performance indicators (KPIs), and maintain open communication for timely issue resolution. Schedule periodic assessments to address risks related to product quality, timely delivery, and regulatory adherence.
- High-Risk Suppliers (Quality-Critical): Carry out comprehensive on-site audits, in-depth evaluations of manufacturing processes, and reviews of quality and safety controls. Maintain close collaboration and implement continuous monitoring to proactively manage and mitigate potential risks.
Conclusion
Supplier qualification is a fundamental part of maintaining compliance and product quality in the pharmaceutical industry. By carefully assessing and monitoring suppliers through comprehensive qualification processes and utilizing tools like Atlas Compliance, pharmaceutical companies can mitigate risks and stay ahead of regulatory challenges.
We provide AI-powered tools and predictive analytics to help pharmaceutical companies qualify suppliers and manage compliance risks effectively. With access to FDA inspection intelligence, regulatory surveillance, and advanced document search capabilities, you can be confident that your pharma supply chain meets the highest industry standards.
Want to learn more about how to optimize supplier qualification? Visit Atlas Compliance to explore our comprehensive compliance solutions or Book a Demo Today!
FAQs
1. How do you qualify as a new supplier in the pharmaceutical industry?
To qualify as a new supplier, companies typically follow six proven methods to ensure quality and compliance:
- Conduct on-site supplier audits
- Verify ISO certifications (e.g., ISO 13485)
- Use detailed supplier questionnaires
- Establish quality agreements
- Perform first article inspections
- Monitor performance with supplier scorecards
These steps help evaluate a supplier’s ability to meet regulatory, quality, and operational expectations before approval.
2. What is vendor qualification, and why is it important?
Vendor qualification is the formal process of assessing and approving suppliers who deliver goods or services. It ensures they meet defined standards for quality, regulatory compliance, and business performance. This process reduces supply chain risks, supports consistent product quality, and strengthens compliance with industry regulations.
3. What does 21 CFR say about supplier qualification?
Under 21 CFR Part 111 (for dietary supplements) and Part 820.50 (for medical devices), the FDA mandates that manufacturers must qualify their suppliers to ensure consistent quality. While the FDA does not specify how to perform the qualification, it expects documented evidence that vendors can reliably meet regulatory and product requirements.
4. What is supplier pre-qualification?
Supplier pre-qualification involves evaluating potential suppliers before entering a business relationship. It includes reviewing the supplier’s financial stability, quality systems, regulatory certifications, manufacturing capabilities, and past performance. Pre-qualification ensures that only capable and compliant vendors proceed to the full qualification stage.
5. What regulatory guidelines govern supplier and vendor qualification?
Several global regulatory guidelines outline requirements for supplier qualification in pharma and medical devices:
- PIC/S Guide to GMP – Part I (Chapters 5 & 7): Covers raw materials, packaging, and outsourced activities.
- PIC/S Guide to GMP – Part II (Chapter 7): Focuses on materials management in pharmaceutical manufacturing.
- ISO 13485 (Clauses 7.4.1–7.4.3): Details requirements for purchasing processes, information, and verification of purchased products.
- FDA 21 CFR Part 820.50: Defines purchasing controls for medical device suppliers, requiring documented evaluation of vendors.
